THE COMPLETE GUIDE TO MAXIMIZING RPM REVENUE AND OUTCOMES
This comprehensive guide aims to provide you with a complete understanding of Remote Patient Monitoring (RPM). It covers a wide range of topics, including:
- Introduction to RPM
- The Advantages of RPM
- How RPM Enhances Telehealth Possibilities
- RPM Reimbursement Explained
- Getting Started with RPM
- Optimizing Your RPM System
- Maximizing Patient Outcomes
- Common RPM Pitfalls and How to Avoid Them
Exploring Recent Developments: Remote Therapeutic Monitoring (RTM)
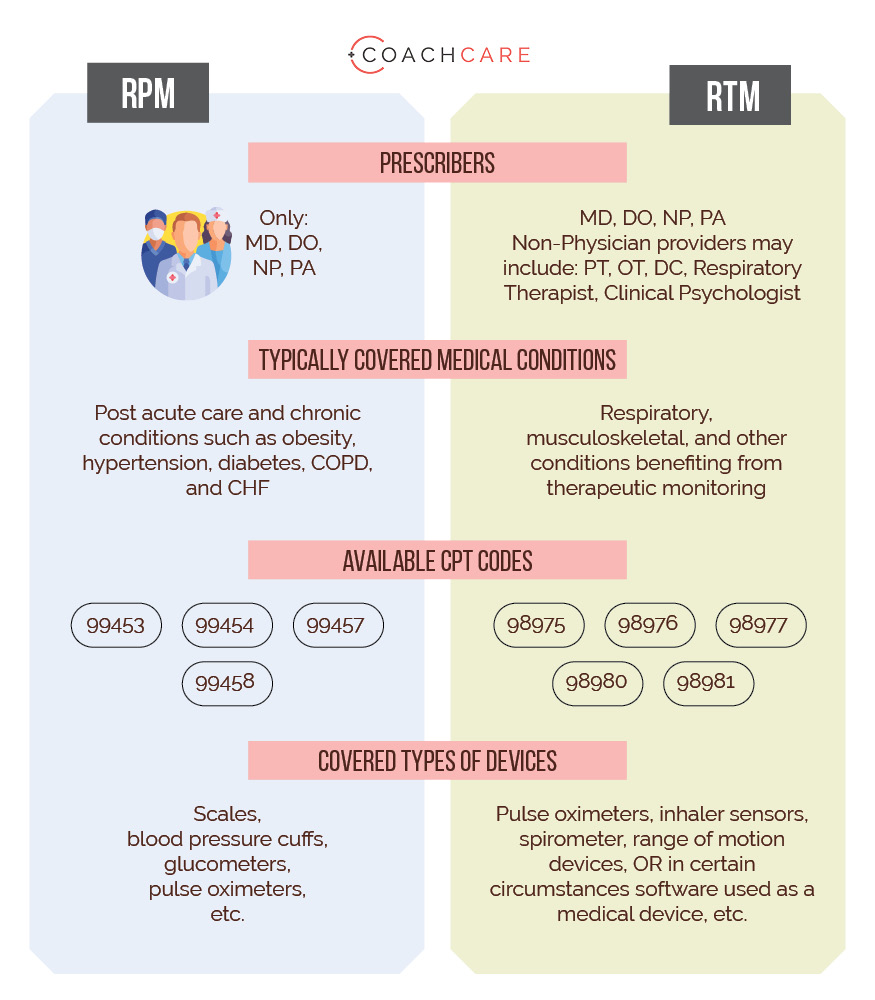
Additionally, we’ll delve into the newly approved reimbursement protocol for healthcare providers like chiropractors, physical therapists, and others, focusing on musculoskeletal conditions, known as Remote Therapeutic Monitoring (RTM). To help you better understand the differences between RPM and RTM, we’ve included a handy comparison chart. For more details on RTM, please refer to our dedicated section here.
Section 1: Introduction to RPM
In recent years, Remote Patient Monitoring (RPM) has gained remarkable traction in the medical community for two compelling reasons:
Enhanced Preventative, Acute, and Chronic Care: RPM offers a more comprehensive approach to healthcare, covering preventative measures, acute situations, and the management of chronic conditions.
Significant Financial Benefits: Healthcare providers have found RPM to be financially rewarding, making it an attractive option for improving patient care.
The concept of caring for patients beyond the physical confines of a medical facility has been evolving, especially in the realm of telehealth. Telehealth consultations, conducted over the phone or via video, have become increasingly prevalent. Recent global events, such as the COVID-19 pandemic, have further accelerated the adoption of telehealth as traditional in-person visits became challenging.
The advent of innovative technologies has empowered healthcare providers to monitor patients’ vital signs and other medical data remotely and in real-time. Thanks to user-friendly software, particularly mobile applications, seamless integration with Bluetooth and Wi-Fi-enabled devices like smart scales, blood pressure cuffs, glucometers, and pulse oximeters has become a reality.
It’s worth noting that the health status of the U.S. population has been on a concerning trajectory, with rising rates of obesity, diabetes, and hypertension. In this context, Remote Patient Monitoring has emerged as an indispensable component of modern patient care.
Section 2: The Advantages of Remote Patient Monitoring
Individuals with chronic health conditions or compromised health are at a heightened risk of experiencing severe symptoms when faced with other illnesses or injuries. The COVID-19 pandemic underscored the vulnerabilities associated with chronic conditions, compelling medical practices to seek innovative solutions. Remote healthcare monitoring systems offer a compelling option with numerous benefits for healthcare providers, patients, and the entire healthcare system.
Boosting Revenue and Profitability
Patients with chronic health conditions often seek home health monitoring solutions, especially with the added risks posed by COVID-19. This presents an opportunity for healthcare providers to generate revenue through Remote Patient Monitoring, with reimbursement codes that can exceed $200 per patient per month.
Efficient Use of Staff Time
RPM streamlines practice operations by delegating tasks related to remote monitoring to junior staff members, freeing up valuable time for nurses and physicians. Automated alerts and escalation features further enhance efficiency.
Reducing Hospital Admissions
By empowering patients to monitor their health at home, Remote Patient Monitoring helps reduce hospitalizations. A study by the Mayo Clinic revealed significant benefits, including greater patient involvement, fewer hospitalizations, fewer ER visits, and cost savings.
Enhancing Patient Outcomes
Managing chronic health conditions requires a different approach than acute conditions. Consistent and timely care can save patients time and money while improving their overall quality of life. In some cases, RPM has led to remarkable results, such as substantial weight loss among participants.
Patient Preference for RPM: Patients appreciate the convenience of RPM, which allows them to access healthcare from the comfort of their homes, eliminating the need for office visits and manual tracking of vital signs. To provide the best RPM services, it’s crucial to offer user-friendly and cutting-edge monitoring solutions.
Key Takeaways
Remote Patient Monitoring is a widely embraced approach that not only boosts practice revenue but also enhances patient care. It reduces emergency room visits, hospital admissions, and improves both the quality and length of life for patients. RPM is an exciting option for healthcare practitioners, offering a range of compelling benefits.
Section 3: Expanding Telehealth Possibilities through Remote Patient Monitoring
The Potential of Telehealth Expanded by CMS
Remote Patient Monitoring (RPM) has revolutionized healthcare by enabling the remote treatment of patients. In addition to telehealth consultations, physicians can now access real-time vital signs data from patients, allowing for proactive intervention rather than discovering issues months or years later.
The Centers for Medicare & Medicaid Services (CMS) recognized the significance of RPM and approved reimbursement for it in 2019. CMS defines RPM as:
“The collection of physiologic data (e.g., ECG, blood pressure, glucose monitoring) digitally stored and/or transmitted by the patient or caregiver or both to the home health agency.”
CMS introduced new Current Procedural Terminology (CPT) codes for RPM, including 99453, 99454, 99457, and 99458. These codes cover various components of RPM, including device and software provision, data monitoring, and patient-provider interactions.
In 2021, CMS provided clarifications regarding RPM, including:
- The necessity of an established patient-physician relationship for RPM services after the COVID-19 Public Health Emergency (PHE) ends.
- The possibility of obtaining consent for RPM services at the time of service.
- Allowing junior staff and contractors to provide RPM services under physician supervision.
- The requirement for FDA-cleared medical devices for RPM services.
- Only eligible physicians and non-physician practitioners (NPPs) for Evaluation and Management (E/M) services may bill RPM services.
Interpreting the CMS Definition
CMS has long recognized the value of remotely capturing patient data. The 99091 CPT code, available for separate reimbursement since 2018, has provided valuable data on the benefits of monitoring patient data. While this code had limitations and was not billable alongside other services, it contributed to CMS’s understanding of data monitoring’s value.
Furthermore, the significant costs associated with emergency room visits and chronic conditions, both in terms of patient well-being and healthcare expenses, have compelled CMS to cover services addressing these issues.
CMS’s description of RPM includes coverage for monitoring various metrics to assist in treating conditions such as obesity, hypertension, pre-diabetes, diabetes, COPD, sleep apnea, prenatal and postpartum care, and pulmonary conditions. For more information on the top three conditions for RPM and specific CPT codes and requirements for billing, please refer here.
Distinguishing Remote Patient Monitoring from Remote Therapeutic Monitoring
Building on the success of RPM, CMS has extended similar services to other specialties through a new set of codes known as Remote Therapeutic Monitoring (RTM). Key differences between RPM and RTM include billing eligibility, covered conditions, and device usage. See below for a comparison between RPM and RTM.
Section 4: Remote Patient Monitoring Reimbursement
CMS has introduced specific CPT codes for Remote Patient Monitoring, and these codes are unbundled, allowing them to be billed in addition to existing E/M codes. CMS relies on CPT codes to ensure precise data capture and accurate claims submission for medical services provided to Medicare and Medicaid beneficiaries.
Understanding CPT Codes
CPT (Current Procedural Terminology) is a standardized coding system created and managed by the American Medical Association (AMA). CPT codes, which consist of five alphanumeric characters, describe various medical services and procedures:
- Category I CPT Codes: 00100-99499
- Category II CPT Codes: 0001F-9007F
- Category III CPT Codes: 0016T-0207T
Usage of CPT Codes
Healthcare professionals across all states use CPT codes to record and describe a wide range of medical services offered to patients. Physicians include diagnoses codes and CPT codes in their documentation when submitting claims to health insurance carriers, whether federal or private.
For physicians and qualified healthcare professionals (QHPs) offering RPM services, a solid understanding of the CPT coding system is crucial for accurate and timely billing. Below, we detail the essential RPM CPT codes:
CPT Code 99453
CPT Code 99453 covers the setup cost of RPM devices and onboarding patients into your remote healthcare monitoring system. This code should be billed once per patient when initiating services.
Key billing requirements include:
- Collecting a patient’s physiologic data for 16 days during a 30-day billing period.
- During the COVID-19 PHE period, billing for code 99453 with less than 16 days of data for COVID-related RPM services.
- Use of an RPM device meeting FDA’s medical device description.
- Physician or QHP orders for RPM treatment.
- Allowance for auxiliary personnel to provide services under physician or QHP supervision.
- Reimbursement rate of $18.84 for both facility and non-facility*.
CPT Code 99454
CPT Code 99454 reimburses providers for supplying patients with home health monitoring devices and programming these devices to record physiologic data. This code should be billed once per patient in a 30-day billing period.
Key billing requirements include:
- Having 16 days of physiological data and/or alerts during a 30-day period.
- During the COVID-19 PHE period, billing for code 99454 with less than 16 days of data for COVID-related RPM services.
- Dispensing RPM devices to patients without additional cost.
- No allowance for patients to bring their devices or lease them.
- Requirement for supplied home monitoring devices to fit FDA’s medical device description.
- Limitation to billing 99454 once in 30 days for all services, even if multiple RPM devices are issued to one patient.
- RPM device orders by physicians or QHPs.
- Allowance for auxiliary personnel to provide services under physician or QHP supervision.
- Reimbursement rate of $48.93 for both facility and non-facility*.
CPT Code 99457
CPT Code 99457 reimburses providers for time spent monitoring, interpreting, and reviewing a patient’s physiological data remotely. This code should be billed once each calendar month.
Key billing requirements include:
- Providing remote health monitoring services for at least 20 minutes per month.
- A live interaction requirement, defined as “real-time two-way remote communication via video, text, email, phone call, and other virtual interactions between you and your patients.”
- Ability to furnish CMS with a patient’s treatment plan and recent data when requested.
- Services performed by QHPs eligible to provide evaluation and management or auxiliary personnel/clinical staff under billing provider supervision.
- Exclusion of text or email as a live interaction; it must be a live video, phone call, or face-to-face conversation.
- Reimbursement rate of $47.61 for non-facility and $31.15 for facility*.
CPT Code 99458
CPT Code 99458 is an add-on code to 99457 and covers each additional 20 minutes of monitoring, with a limit of up to three units per calendar month based on medical necessity.
Key billing requirements include:
- Billing 99458 only as an add-on to 99457, not as an independent code.
- Services performed by QHPs eligible to provide evaluation and management or auxiliary personnel/clinical staff under billing provider supervision.
- The reimbursement rate is $38.68 for non-facility and $31.15 for facility.*
* These are average Medicare rates. Actual reimbursement varies by MAC locality. Private payers set their own rates and are not required to reimburse at the rates set by Medicare.
Section 5: How RPM Reimbursements Function
In order to receive compensation for the remote healthcare monitoring services you provide to patients, it’s imperative to adhere to CMS billing rules. RPM reimbursement rates may vary among private insurance companies, but they typically align with the rates established by CMS. When CMS updates reimbursement figures, they are published in their annual Physician Fee Schedule report.
Unlocking Your Revenue Potential with RPM
Enhanced financial performance translates into improved patient care. Remote Patient Monitoring (RPM) stands as one of the most promising revenue streams for established healthcare practices.
To recap, here’s a summary of RPM reimbursement rates:
- CPT 99453: $18.84 (one-time)
- CPT 99454: $48.93 (monthly, for passive data collection)
- CPT 99457: $47.61 (monthly, if actively monitored)
- CPT 99458: $38.68 (monthly, if actively monitored)
- CPT 99458 (additional units): $38.68 (monthly, if actively monitored)
This equates to a minimum monthly revenue of $48.93 for every patient enrolled in an RPM program. This minimum reimbursement requires no staff time and serves as compensation for passive data collection.
The maximum reimbursement potential is $196.44. To achieve this maximum reimbursement, clinical staff must actively monitor patients and conduct at least one consultation per patient, spending a total of 60 minutes during the calendar month.
It’s important to note that RPM codes are unbundled, allowing practices to bill for other services, such as telehealth and chronic care management, without any restrictions.
Smaller practices typically generate around $250,000 in new annual revenue through RPM, while larger physician groups and health systems can anticipate $1,000,000 or more in new revenue. To estimate the revenue impact RPM can have on your practice, you can use this RPM calculator.
Section 6: Tips for Ensuring CMS Compliance in Your Practice
Outsource Administrative Tasks
A prudent approach is to outsource your RPM administrative tasks to your RPM platform provider. These tasks encompass documenting patient data, securing patient consent, setting up and onboarding both patients and staff on your remote health monitoring system, and supplying RPM devices to your patients.
Select the Right RPM Devices
Ensuring a seamless user experience with wearable health monitoring devices for your patients is crucial. This facilitates the effortless transmission of physiological data with minimal downtimes. As a prerequisite, the devices used for RPM must meet FDA medical-grade standards, distinguishing them from consumer-grade alternatives. For detailed insights into device options for RPM, you can refer to this comprehensive review.
Identify the Ideal Patient Population
Patients with acute conditions and those managing chronic conditions like diabetes, heart disease, and hypertension stand to benefit the most from remote patient monitoring services. These individuals provide an opportunity to collect daily physiological data, and it’s essential to educate them on effectively using their RPM devices to gather and transmit data. This proactive approach enables remote health monitoring and ensures the accumulation of sufficient data to meet billing requirements.
Additionally, it’s crucial to have a comprehensive understanding of each patient’s insurance coverage. Conducting a benefits eligibility check before prescribing RPM is considered a best practice.
Section 7: Initiating Your RPM Journey
Embarking on the path of Remote Patient Monitoring (RPM) might seem like a monumental task for your practice, but the truth is, with an experienced vendor, it can be accomplished in just 3-4 weeks and require less than 6 hours of staff time.
The RPM implementation process encompasses the following steps:
- Select a Vendor
- This choice is pivotal, so opt for an RPM vendor with substantial experience in the field.
- Look for vendors with at least five years of remote monitoring experience and a substantial user base, preferably over 100,000 patients.
- Seek vendors who can provide numerous testimonials and referrals.
- Ensure the vendor offers free access to their platform for testing.
- Live training for your staff is essential, and the vendor should be capable of addressing all your inquiries in detail.
- The presence of coding and billing experts on the vendor’s team is crucial.
RPM Devices:
To ensure the successful delivery and billing of RPM services, the devices placed in patients’ homes must be FDA-cleared and of medical-grade quality.
It’s crucial that these devices are provided by the prescribing physician, and patients should not use their own devices.
RPM vendors should offer fully integrated devices and avoid off-the-shelf products like FitBit. RPM vendors must not merely procure devices from other companies, as this can compromise data reliability and patient compliance.
Device Connectivity Options:
There are three connectivity options for RPM devices: Bluetooth, cellular, and base station.
Bluetooth
These devices connect directly to a mobile app on a patient’s phone, offering a straightforward setup. Bluetooth devices are cost-effective and promote patient engagement by requiring interaction with the mobile app.
Cellular
Cellular devices transmit data automatically via cellular networks, simplifying ongoing usage. However, they are more expensive initially and involve ongoing data costs.
Base Station
This option is the most complex and costly but beneficial for very old or seriously ill patients needing multiple devices.
For further insights into RPM devices, you can refer to this informative article.
Section 8: Maximizing the Potential of Your RPM System
Launching an RPM program is an exciting endeavor that can bring about dramatic changes in your practice and patient care. Here’s how to ensure you get the most out of your RPM program:
Vendor Selection
Choosing the right RPM software/hardware vendor is paramount to your program’s success. Refer to the discussion above for guidance on what to look for in RPM vendors.
- Consider your specific needs, such as whether a general RPM platform or one tailored to your specialty is more suitable. Decide if you’ll handle monitoring or outsource it to your RPM vendor.
- Assess the level of support required for claims and billing.
- Take into account the technology needs of your patients.
Launch Plan
A strategic launch plan is instrumental in ensuring a smooth rollout and rapid patient enrollment into the RPM program.
Collaborate with your RPM vendor to create a comprehensive launch plan that includes implementation schedules, patient identification processes, scripts for patient communication, and an implementation team responsible for various aspects of the process.
Your Responsibilities
Success in your RPM program depends on leadership commitment, with the head of the practice or department making RPM an integral part of patient care.
Designate a point person within your practice responsible for implementation.
Establish standard operating procedures for identifying eligible patients and presenting RPM as an option to them.
Key Takeaways
Collaborating with the right vendor, devising a well-thought-out launch plan, and actively participating in the process are key to the success of RPM programs.
If you’re not fully prepared for RPM implementation, it’s better to wait until you and your practice are ready rather than rushing into it with lower chances of success.
Section 9: Achieving Optimal Outcomes
Remote Patient Monitoring (RPM) represents a remarkable opportunity to elevate the quality of care provided to patients and enhance medical outcomes significantly. RPM enables a shift from episodic care to proactive care based on patient needs, emphasizing prevention and early intervention.
Enroll Patients at the Population Level
Initially, it’s valuable to enroll as many eligible patients as possible to create a meaningful impact across the population.
Gathering data on a large scale allows for more effective triage and maximizes revenue potential.
Harness Alerts & Escalation
Setting up alerts and escalation protocols is crucial for identifying patients in real-time who require assistance.
The software processes data and pinpoints patients needing intervention, enabling the immediate treatment of developing conditions.
Early & Precise Interventions
When alerted to a patient’s needs, you can swiftly take action.
Review available data to make informed treatment decisions, such as medication adjustments, or schedule consultations with patients.
Often, you can identify issues before speaking with the patient, streamlining explanations and solutions.
Key Takeaways
Employ RPM with a population-focused approach to impact patient care effectively.
Leverage software to generate alerts and escalations.
Intervene precisely and promptly when necessary.
Section 10: Avoiding Common RPM Pitfalls
Strategic implementation is just as crucial as selecting the right approach. Learning from common mistakes made by providers can save you time and resources. Some pitfalls to avoid include:
Choosing the Wrong Vendor
- Avoid vendors with less than five years of experience or fewer than 100,000 patients.
- Be cautious if the technology appears outdated.
- Ensure you interact with key support staff, not just salespeople.
- Select vendors knowledgeable about CPT codes and billing processes.
Lack of Commitment
RPM should only be adopted when you’re ready to make it a priority in your practice.
Ensure all staff align with this commitment to avoid wasted resources.
Missing Reimbursements
- Some CPT codes have specific time requirements; ensure staff meet these to maximize revenue.
- Educate your billing team about RPM codes and documentation.
- Address denials thoughtfully, often a minor change can result in payment.
Disclaimer
It’s important to consult with professionals for specific advice tailored to your circumstances, as this information is for general purposes only.

